Microbial contamination is a growing concern
The transfer of pathogens to a patient from a contaminated device, potentially leading to infection, is a risk of all endoscopic procedures.1 Flexible endoscopes have been associated with more outbreaks of infection than any other reusable medical or surgical device.1
Compliance with reprocessing guidelines is crucial to lower the risk of contamination.1 However, multiple studies have reported that endoscopes can be contaminated with potentially pathogenic microbes even when cleaning and reprocessing guidelines are strictly followed2-4
Improperly reprocessed endoscopes have been linked to outbreaks
Over 200 journal articles were published in the last decade involving contamination, cleaning failure, or infections associated with flexible endoscopes.
Incidents of contamination have been reported for all major endoscope types.

Manual cleaning is the most important step of reprocessing
Endoscope reprocessing is a highly complicated process that can include dozens of individual steps.
Of these steps, the manual brushing and flushing of endoscope channels is recognized as the most critical for successful reprocessing.6

Manual cleaning is often not effective
Manual cleaning is today’s gold standard, but has key problems that need to be addressed. Failure of reprocessing just due to inadequate manual cleaning is well documented.3
In a prospective observational study, 92% of endoscopes had protein or ATP levels that exceeded benchmarks after manual cleaning, indicating contamination. This was despite adherence to the site’s cleaning protocols and reprocessing guidelines.7

- Rutala, W. A. & Weber, D. J. Reprocessing semicritical items: Outbreaks and current issues. Am J Infect Control 47, A79–A89 (2019).
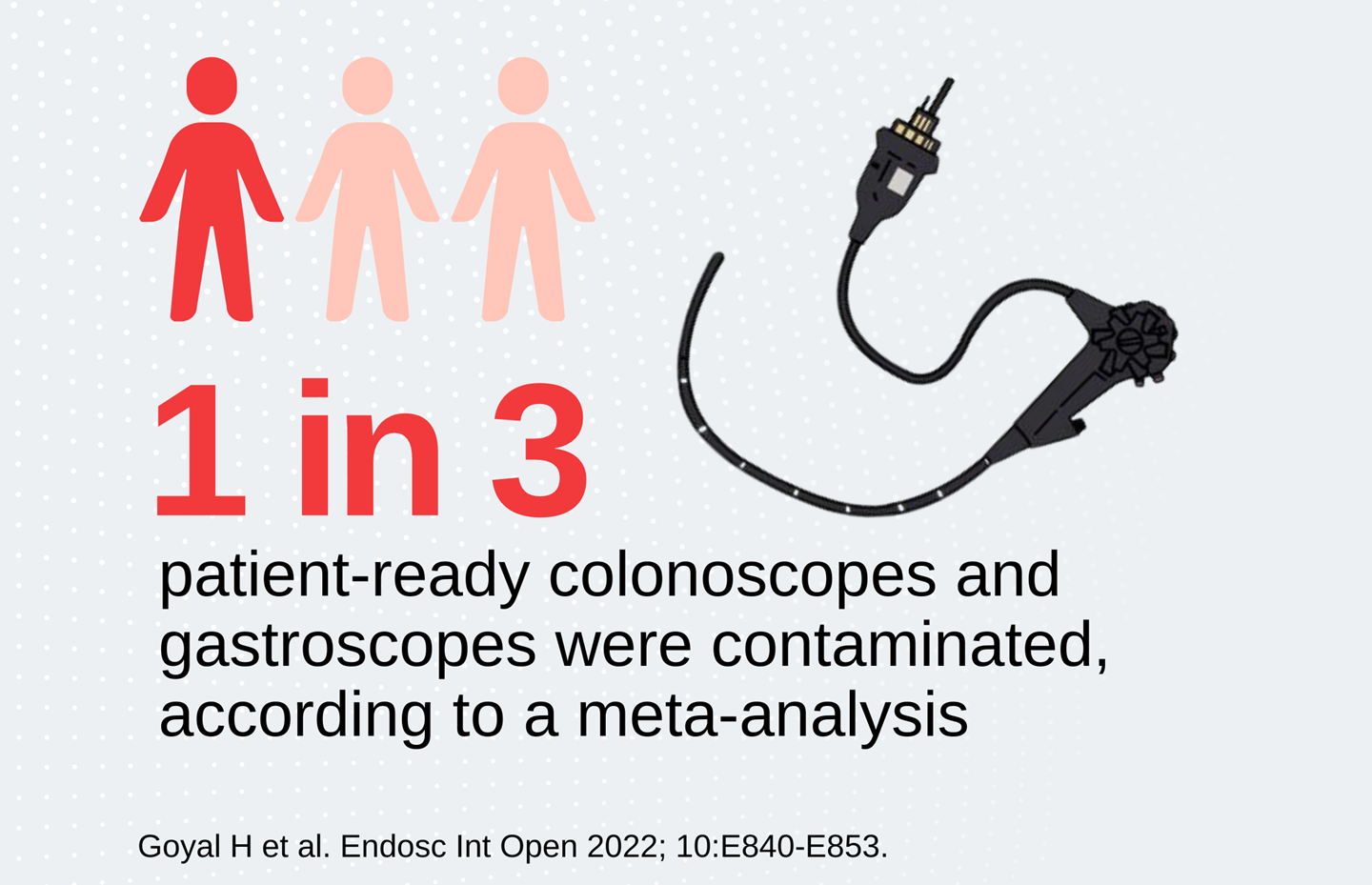
- Goyal H et al. Gastrointestinal endoscope contamination rates – elevators are not only to blame: a systematic review and meta-analysis. Endosc Int Open 2022; 10: E840–E853
- Ofstead CL et al. Challenges in achieving effective high-level disinfection in endoscope reprocessing. Am J Infect Control. 2020 Mar;48(3):309-315. doi: 10.1016/j.ajic.2019.09.013. Epub 2019 Oct 31.
- Johani K et al. Determination of bacterial species present in biofilm contaminating the channels of clinical endoscopes. Volume 23, Issue 4, December 2018, Pages 189-196.
- Kovaleva, J., Peters, F. T. M., Mei, H. C. van der & Degener, J. E. Transmission of Infection by Flexible Gastrointestinal Endoscopy and Bronchoscopy. Clinical Microbiology Reviews 2013; 26(2):231–254.
- Gastroenterological Nurses College of Australia. (2021). Infection Prevention and Control in Endoscopy 2021. https://www.genca.org/public/5/files/Nurses%20info/IPCE%202021_Feb2022update.pdf
- Ofstead CL, Wetzler HP, Doyle EM, Rocco CK, Visrodia KH, Baron TH, et al. Persistent contamination on colonoscopes and gastroscopes detected by biologic cultures and rapid indicators despite reprocessing performed in accordance with guidelines. Am J Infect Control 2015;43:794-801.

